What is a stress fracture?
A bone can crack because of repetitive intermittent pressure, just as concrete can. Any repetitive activity can cause a stress fracture, and any bone in the body which is subjected to repetitive stress can suffer this injury. The damage is caused not just by repetitive impact, but through the pulling or shearing action of muscles and tendons against the bones.
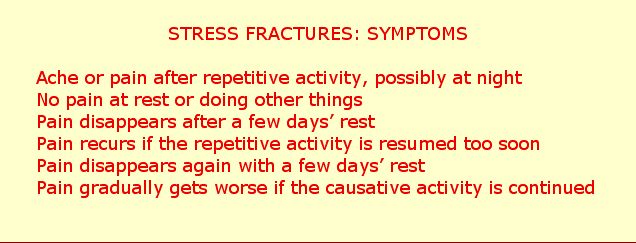
The injury in always gradual, starting as a niggle or ache. Technically this is known as “insidious onset”. Typically, there is pain only after the activity at first, often overnight. The pain becomes more obvious, if the activity which caused it is continued. As the problem gets worse, pain is felt during the activity, although it may be quite mild. Later it may become bad enough to put a stop to the activity, eventually becoming noticeable while doing other things involving the injured area. At every stage, the pain disappears with rest, but it comes back increasingly quickly and severely if the causative activity is resumed too soon, before full healing has taken place.
How is a stress fracture different from other types of bone break?
In a traumatic fracture, there is always an obvious cause. The pain and other symptoms of the broken bone are felt immediately or shortly after the accident, and the fracture usually shows up straight away on X-ray.
A stress fracture is never related to a single incident, and X-rays are almost invariably clear in the early stages. The first X-ray evidence of the fracture is usually later, when there is a “cloud” of healing bone, technically callus, around the fracture site.
A traumatic fracture hurts whenever pressure is applied over the area, until it has healed completely, and sometimes even after that. A stress fracture quickly becomes painless if the activity which caused it is stopped, even before the bone has healed.
A traumatic fracture heals progressively with protection or immobilization in a cast, so long as there are not any complicating factors such as infection which prevent or delay healing. If a stress fracture is immobilized in a rigid cast, it does not heal. If the stress fracture is not properly treated, it can remain present for months or even years, getting neither worse nor better. If activities which cause pain over the fracture site are continued, the fracture will get worse. The pain will increase, and in some cases the bone might snap completely.
The first London Marathon in 1981 saw thousands of people take to the streets to participate, many with no experience of marathon running and with inadequate training. The most serious injury on that occasion was a male runner who tried to take part despite a nagging pain in his thigh: in fact it was a stress fracture in the thigh-bone, and the bone broke right through late in the race, so he finished up in hospital. Typically, the pain had not been severe enough to warn the runner that he might have a potentially serious injury.
The indications may be clear enough to provide reasonable certainty that the injury is a stress fracture, so the recovery programme can be started straight away.
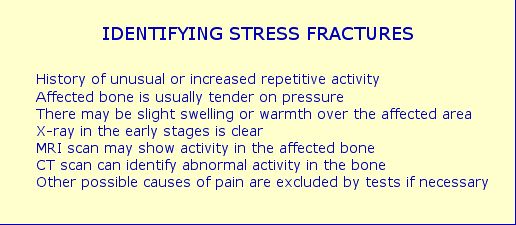
If there is any doubt about the diagnosis, your doctor or specialist might request a CT or MRI scan of the bone. Tests may also be done to exclude any other possible reasons for your symptoms.
Technical definitions
Stress fractures have been classified in two main groups, distraction and compression fractures, according to the type of pressure which causes the injury and their appearance on X-rays.
Distraction fractures can be subdivided into three groups: transverse, running horizontally across the bone, longitudinal, running vertically, and oblique, extending diagonally.
The initial bone damage in a stress fracture has been identified as a breakdown of the tiny crystals, technically known as hydroxyapatite crystals, which form the hard mineral part of the substance of the bone.
Why do stress fractures happen?
Our bones are only as strong as they need to be for our normal activities. Bones adapt and strengthen according to the demands made of them. This is why appropriate exercise is so important for maintaining bone health as we get older, or at times like the menopause in females when the bones can tend to weaken. Bone strength is naturally affected by our diet, so it is advisable to eat foods which help maintain good calcium levels, and to avoid substances such as the fizzy drinks which are known to deplete calcium.
To prevent stress injuries, one has to understand how the body reacts to repetitive movement. Any unusual repetitive stress can cause a bone to crack under pressure. All it takes is an increase in the amount we do of a repetitive activity, sometimes, but not always coupled with weakening in our bones due to other factors. Impact is not necessarily a factor. Stress fractures can happen in bones which do not transmit shock directly, such as the kneecap and the fine bones at the sides of the vertebrae. Running on soft surfaces like grass or cross-country does not necessarily prevent stress fractures.
A stress fracture rarely happens through a single session. It’s certainly possible for a bone to be damaged through a bout of unusual and prolonged repetitive activity, but if it’s a one-off the bone will normally heal and not cause problems.
For a stress fracture to occur and cause problems, the repetitive activity has to be done over a space of days or weeks, without allowing sufficient rest days for the bones to adapt to the increased workload. Micro-trauma often occurs in our bones due to repetitive stress. In the normal way, the bones recover and become stronger as a result, but if they are subjected to more stress than they can cope with, they can start to crack.
There is no hard and fast rule about how much repetitive activity is needed to cause damage: it varies according to the state of the bones involved, and can happen surprisingly quickly and easily. Our bones can be relatively weak simply through lack of exercise in sedentary people who take no exercise, more so if there has been a period of bedrest for any reason. Bones are obviously even more vulnerable if they are weakened or osteoporotic due to mineral deficiency, hormonal influences or disease. Most studies of comparable groups show that females are more prone to stress fractures than males.
What activities cause stress fractures?
Foot and leg stress fractures are the most common, and are prevalent among walkers or runners, whether athletes, military recruits or non-sporting individuals. The injury is always associated with a change in routine. A sedentary person who goes unprepared on a walking holiday covering several miles day after day can suffer leg stress fractures after only a few days. In runners, the change might be an increase in mileage during running training; re-starting running on a daily basis after a lay-off; or starting a running programme from scratch and running every day or almost every day.
The first known formal studies of stress fractures, dating to over 150 years ago, were on military recruits who were suddenly doing a lot of marching day after day. The stress fractures seen in the metatarsal bones of their feet (the long bones leading to the toes), which most commonly affected the second metatarsal, were therefore called “march fractures”.
Stress fractures from running too much can affect not only the foot, but also the shin, the fibula (outer leg-bone), thigh-bone (femur) and the more delicate bones of the pubis. The term “shin splints” is a vague definition covering all causes of pain in the front of the lower leg, but very often the injury is a stress fracture of the shin-bone (tibia).
Skipping, jumping, hopping and bounding can also lead to foot and leg stress fractures, if you do unusual amounts of these on a daily or near-daily basis. This is a hazard of ballet dancing. Competitive high jumpers in intensive training can suffer stress fractures in the small bones of the mid-foot through the particular pattern in which they twist over the foot during take-off.
While foot and leg stress fractures are the most common, the injury can affect any of the body’s moving parts. For instance, sports involving repeated twisting movements in the trunk, such as the throwing events, rowing and fencing can lead to stress fractures in the ribs or spinal bones.
Activities which involve varied movements, and which should not normally cause stress fractures, can be made repetitive enough to cause the injury. Excessive amounts of service practice or fixed drills in tennis can lead to stress fractures in the spinal bones or the arm. Drills to practise one shot and a particular pattern of movement in squash can cause stress fractures in the kneecap.
Stress fractures don’t only happen to sports players. An unaccustomed stint of physical activities like hiking, chopping wood or digging the garden on consecutive days can lead to the injury in the relevant parts of the body.
How are stress fractures cured?
There are three priorities:
1. Avoid any pain-causing activities.
2. Rest from the causative activity or any pain-causing activities long enough for the bone to heal.
3. Stimulate the blood flow in the affected area to help the bone to heal.
The injured area should be protected, if it causes pain during normal activities. For the foot or leg a removable cast may be used, for the arm a wrist brace or sling if necessary. If there is generally no pain, it is best not to restrict movement. Painless normal activities should be continued, and you should avoid sitting or standing still.
Any painless general exercise, such as working with weights machines, free exercises, yoga, swimming and cycling will help the body’s blood flow and therefore help healing, as well as keeping you fit overall.
Hot and cold bathing and gentle massage around the injury with arnica or heparinoid cream will help promote the local blood flow, as does rolling the sole of the foot over a golf ball, or using Chinese iron balls for hand exercises. These techniques help control any localized swelling, and can be repeated two or three times a day, provided there is no adverse reaction of any kind.
It is vital not to return to the causative activity too soon. As a rule of thumb, stress fractures in the finer bones, such as the foot, outer leg-bone (fibula), wrist or arm need at least six weeks' rest from the causative activity, while the major weightbearing bones like the shin-bone and thigh-bone should be given eight to twelve weeks. There has to be a defined period when there is no pain at all in the injured area before a return to repetitive activities can be considered. It is usually possible for an experienced practitioner to tell when healing has taken place by pressing over the bone, and taking into account the absence of swelling or localized warmth. If there is any doubt, check X-rays or scans may be advisable.
Most stress fractures heal without any problem, if they are given time, and the healing processes are helped along as described above. Rarely, the injured bone might fail to heal, and then an operation may be needed to fix the bone or to stimulate bone healing. It may also be necessary to have tests to identify whether there is mineral deficiency from any cause.
In order to avoid a recurrence of the problem or a secondary injury, you have to resume repetitive activities on a very gradual basis. For runners, for instance, I recommend running a short distance once a week for the first month, twice a week for the second month, three times in the third month, and then a gradual build-up of distance and speed over the next three months. It's best to run on a mixture of hard and softer surfaces, not just to reduce impact, but to allow for different patterns of muscle work. On a softer surface, the foot moves more variably, and causes slight changes in the action of the tendons and muscles against the bone. Avoid heavily cushioned shoes which impede normal foot movements: it's best to wear flexible shoes with a protective soft cushioning insole, to allow for natural foot movement. The distance run in the first session should be comfortable. The important part is the rest in between sessions. if you feel any stiffness or ache after a session, on no account should you run again until the symptoms have subsided completely.
The same principles apply to returning to sports other than running, after a stress fracture in the arm or a spinal bone. Sessions should be well spaced out, with a gradual increase in activity and frequency over a space of months.
If at any time there is pain following a session, you have to rest for at least a week, possibly more, until all the symptoms have disappeared. Then you can resume, but doing less than you had built up to. You may even need to go back to the schedule for the first month and re-start the whole process.
From the start of your rehabilitation programme, you should be doing cross-training using different types of exercise. It’s advisable to keep doing protective exercises and fitness conditioning work even when you are fully recovered.
To prevent stress fractures, I strongly advise against doing a particular sport more than three, maximum four, times a week especially if it involves repetitive movements; never make a sudden increase in your physical activities or sports programme; re-start sports gradually after a lay-off; vary your physical activities as much as possible; allow rest days between sessions involving repetitive movements; eat healthily; and never ignore warning signs such as pain relating to activity.
© Vivian Grisogono 2008. Updated 2014